Prostatectomy
Surgery for Localized Prostate Cancer – Weighing Your Options
Men who have been diagnosed with prostate cancer typically have many questions. That is certainly understandable. Perhaps the most common question: What can you expect from treatment?
Treatment decisions are often based on the extent of the cancer. The term localized is used to describe prostate cancer that hasn’t spread outside the prostate gland. Another term for localized cancer is organ-confined cancer.
A cancer diagnosis typically includes a discussion of cancer stages– the degree to which the cancer has progressed. Here’s an overview:
Stage 1.
Stage 1 is the earliest stage of prostate cancer, when cells are not growing as quickly. The tumor can’t be detected during a digital rectal exam (DRE).
Stage 2.
During stage 2, the tumor is confined to the prostate gland. The tumor might be detected during a DRE. At this stage, the cancer is still found only in your prostate gland, but the risk of it growing and spreading to other areas is higher.
Stage 3.
During stage 3, the tumor is growing. At this point, it is likely to continue to grow and may begin to spread, even to other areas of the body, like the seminal vesicles (glands that produce seminal fluid), bladder, or rectum.
Stage 4.
At stage 4, cancer has spread outside the prostate gland. It is no longer localized.
Treatment decisions are often based on the extent of the cancer.
Localized prostate cancer is treated in several ways. A combination of treatments may be recommended. Here are some examples:
- Active surveillance involves monitoring the cancer through regular tests. Treatment begins if and when necessary.
- Watchful waiting is a wait-and-see approach similar to active surveillance. However, regular testing is not done.
- Radiation therapy uses high energy rays to destroy cancer cells or slow down their spread.
- Hormonal therapy (also called androgen deprivation therapy or ADT), cuts the supply of testosterone and other male hormones that fuel the growth of prostate cancer cells.
- Cryotherapy (cryoblation) destroys cancer cells by freezing them.
Surgery is another option.

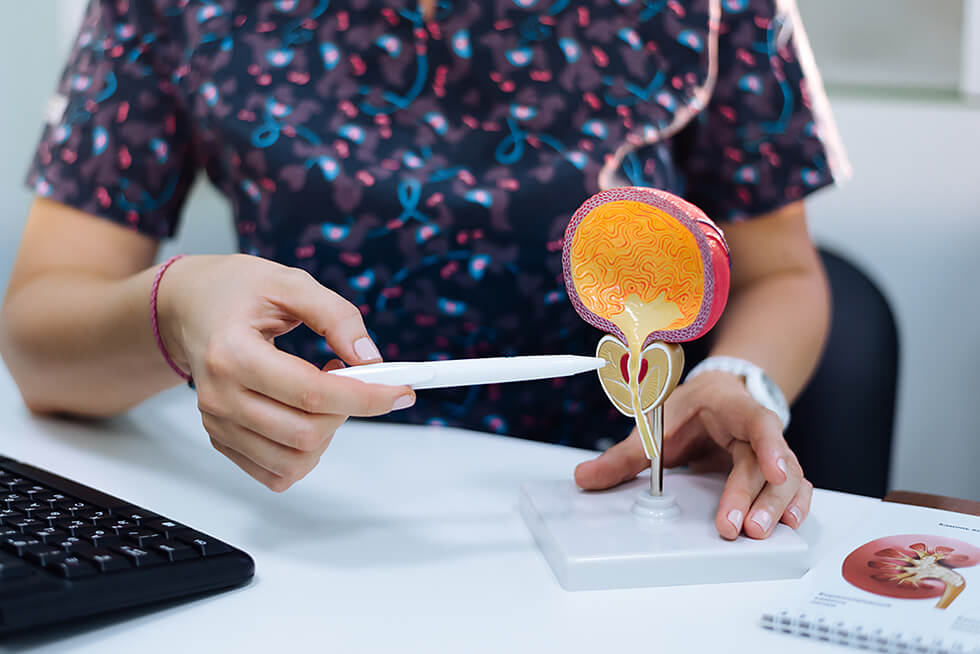
The surgical procedure for treating localized prostate cancer is called a radical prostatectomy, and it involves removing the entire prostate, seminal vesicles, and some surrounding tissue. Sometimes, lymph nodes are also removed.
By far, the most common procedure is robot-assisted laparoscopic prostatectomy (RALP).
Robotic surgery is routine nowadays
In laparoscopic procedures, about 6 small 1- to 2-inch incisions are made in the abdominal wall. These incisions are called “ports,” and they provide access for surgical instruments. One of the instruments, the laparoscope, includes a tiny camera that guides the surgeon’s movements.
With a robotic procedure, the surgeon sits at a computer monitor and controls the movements of a robot that holds the instruments. Robotic surgery is routine nowadays, and surgeons using this technology receive thorough training.
Laparoscopic prostatectomies can be done without robots, too. In a traditional laparoscopic procedure, the surgeon holds the instruments.
In rare cases, an open prostatectomy is performed. In an open procedure, the surgeon will remove the prostate through one long incision (about 8 to 10 inches). Usually, the incision is between the belly button and pubic bone (called a radical retropubic prostatectomy) or between the anus and scrotum (a radical perineal prostatectomy).
No matter the type of surgery, there are two potential key complications to prepare for:
Erectile dysfunction (ED)
ED is difficulty getting and keeping an erection rigid enough for intercourse. It’s not uncommon after prostate cancer surgery. That’s because the prostate gland is surrounded by nerves that are essential for erectile function. While surgeons take care to preserve as many nerves as possible, some nerve damage can occur.
Often, men undergo nerve-sparing procedures. In these cases, the surgeon takes special measures to keep erectile nerves intact. Research suggests that nerve-sparing surgeries have better erectile function outcomes than non-nerve-sparing procedures.
Many men find their erectile function improves over time, but recovery will likely require patience. It can take up to two years after surgery to see sustained progress in erectile firmness. Fortunately, there are several treatments for ED.
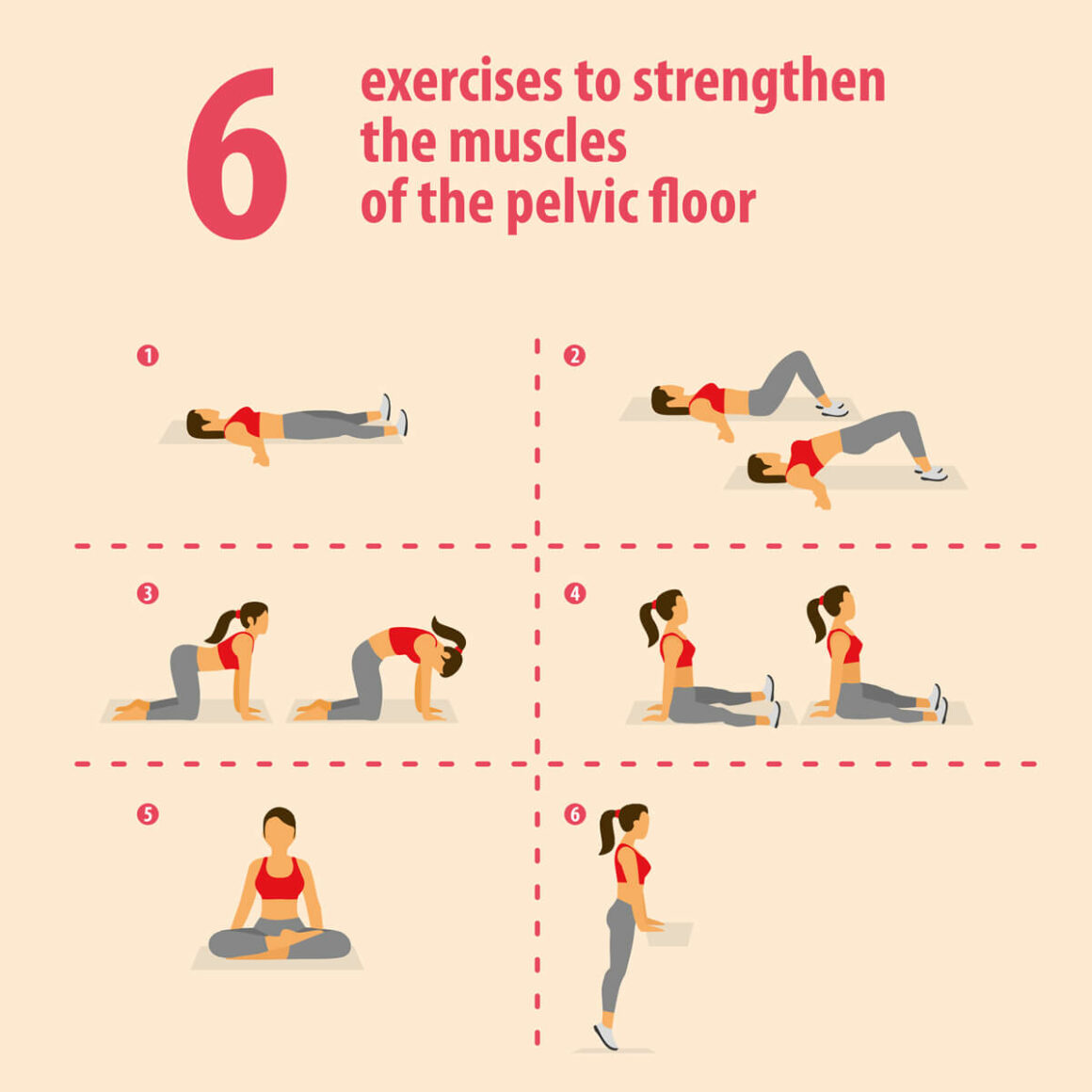
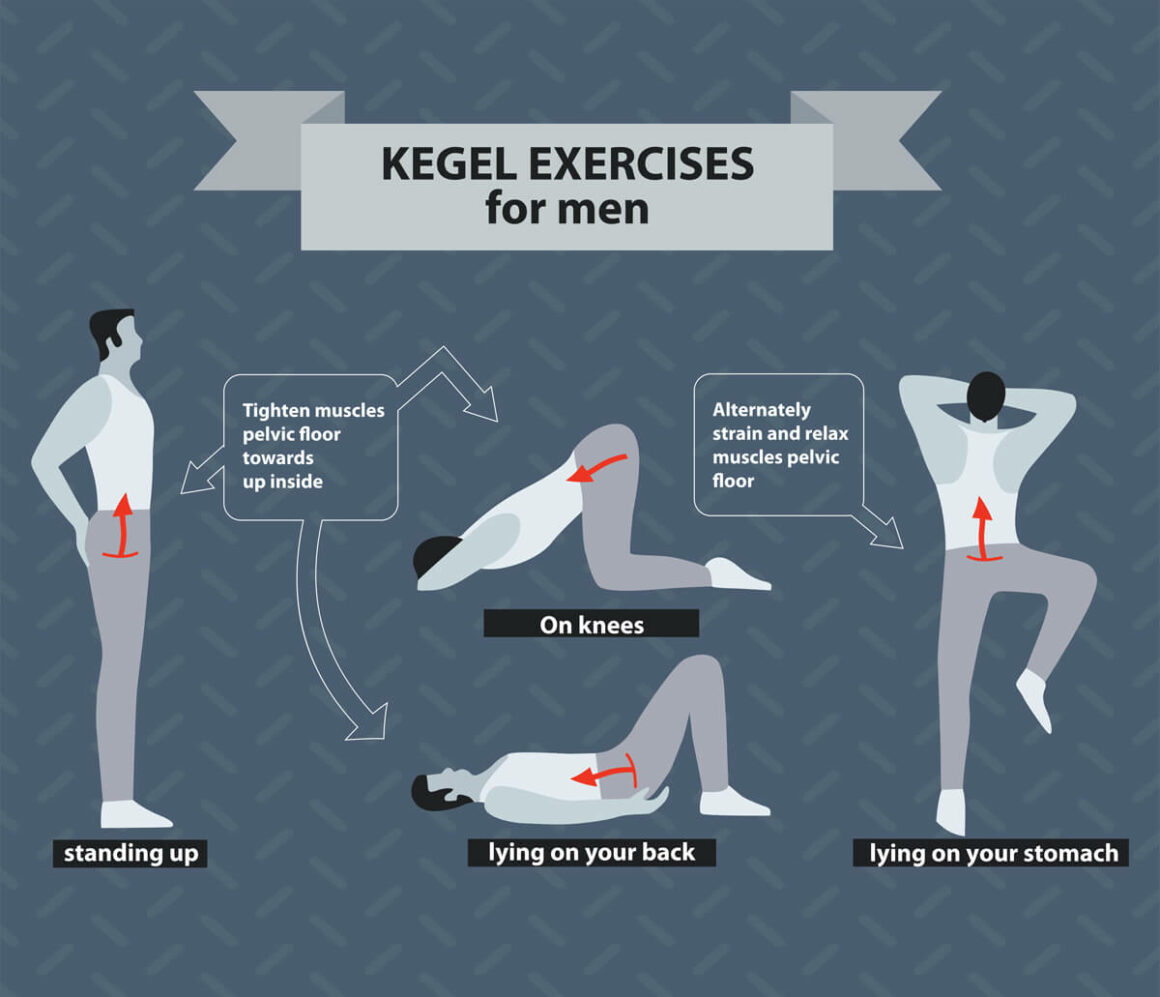
Incontinence
Leaking urine after prostatectomy is quite common. It might be difficult to empty your bladder, or urine might leak when coughing or working out. Some men feel like they have to urinate right away. This side effect usually goes back to normal within a few months, but it can be frustrating while enduring it. Various assistive and therapeutic strategies are available.
Older men are more likely to have trouble with erections or incontinence than younger men. However, both conditions can be treated in men of all of ages.
Is Robot-Assisted Laparoscopic Prostatectomy (RALP) Better Than Open Prostatectomy?
Not necessarily. All types of surgery are effective for removing the prostate gland and treating prostate cancer. And the sexual and urinary side effects are similar for all approaches.
However, laparoscopic approaches do have some advantages over open prostatectomy:
- They’re less invasive.
- They use smaller incisions, which heal more quickly.
- There is typically less bleeding and less pain.
- Most men have shorter hospital stays (usually about a day or two, compared to a few days with open prostatectomy).
- Men are catheterized for a shorter period of time. (A catheter is a thin tube that allows urine to flow from the bladder to a collection bag.)
How about robotic vs. traditional laparoscopic prostatectomy? Research presented in 2020 suggests that men who have robotic procedures have better bladder control after surgery. Future research may shed more light on this issue.
The decisions we make with our patients about their treatment path require processing and understanding a good deal of information. Questions are always welcome. Comprehensive support will be provided both before and after surgery.
Resources
American Cancer Society
“Surgery for Prostate Cancer”
(Last revised: August 1, 2019)
https://www.cancer.org/cancer/prostate-cancer/treating/surgery.html
American Urological Association
Sanda, Martin G., et al.
“Clinically Localized Prostate Cancer: AUA/ASTRO/SUO Guideline (2017)”
(Published: 2017)
https://www.auanet.org/guidelines/guidelines/prostate-cancer-clinically-localized-guideline
American Society of Clinical Oncology (ASCO)
“Prostate Cancer: Stages and Grades”
(Approved by Editorial Board: November 2019)
https://www.cancer.net/cancer-types/prostate-cancer/stages-and-grades
“Prostate Cancer: Types of Treatment”
(Approved by Editorial Board: November 2019)
https://www.cancer.net/cancer-types/prostate-cancer/types-treatment
Medscape Medical News
Freeman, Sara
“Better Continence Rate Gives Robotic Prostatectomy the Edge”
(August 5, 2020)
https://www.medscape.com/viewarticle/935215
National Cancer Institute
“Prostate Cancer Treatment (PDQ®)–Patient Version”
(Updated: June 26, 2020)
https://www.cancer.gov/types/prostate/patient/prostate-treatment-pdq
Urology Care Foundation (American Urological Association)
“Insights: Radical Prostatectomy”
(Winter 2018)
https://www.urologyhealth.org/patient-magazine/magazine-archives/2018/winter-2018/insights-radical-prostatectomy
“What is Prostate Cancer?”
(Updated: January 2020)
https://www.urologyhealth.org/urologic-conditions/prostate-cancer
“What You Should Know About Surgery for Prostate Cancer”
(2018)
Downloadable PDF via https://www.urologyhealth.org/urologic-conditions/prostate-cancer#Surgery
UpToDate.com
Klein, Eric A., MD
“Patient education: Prostate cancer treatment; stage I to III cancer (Beyond the Basics)”
(Topic last updated: January 8, 2019)
https://www.uptodate.com/contents/prostate-cancer-treatment-stage-i-to-iii-cancer-beyond-the-basics