Low Testosterone/Testosterone Deficiency
Testosterone is the reason males develop characteristics like facial hair and a deeper voice. It drives a man’s libido and helps with erections. It’s also involved with sperm production, muscle strength, and bone health. Produced by the testicles, testosterone is what’s known as an androgen—a hormone responsible for masculine traits. (Note: While women’s bodies produce testosterone in smaller amounts, it is usually considered a male hormone.)
Sometimes, men don’t produce enough testosterone (this is called hypogonadism or “low testosterone”)
Sometimes, men don’t produce enough testosterone (this is called hypogonadism or “low testosterone”). This may happen due to a congenital condition (something a man is born with), an injury, cancer treatment, or other reasons. In addition, men’s testosterone levels decline as they get older.
When low testosterone is accompanied by other symptoms, like low sex drive, fatigue, and moodiness, urologists make a diagnosis of testosterone deficiency (TD).
The Urology Care Foundation estimates that 2% of men have TD. It is more frequent in older men, overweight men, and men with diabetes.
What are the symptoms of testosterone deficiency?
The typical symptoms of TD include the following:
Less interest in sex
Erectile dysfunction
Fatigue
Moodiness, depression, or irritability
Loss of muscle mass
Weaker bones
Less body or facial hair
Development of breasts (gynecomastia)
TD symptoms are similar to symptoms of other conditions. For example, trouble with erections can be a sign of diabetes or heart disease. Low sex drive could be linked to depression or be a side effect of medication. For these reasons, it’s a good idea to call your doctor if you have any of these symptoms so you can have a thorough medical exam.
What causes testosterone deficiency?
Congenital conditions
These are medical conditions that you’re born with. On example is Klinefelter syndrome, when a genetically male child is born with an extra X chromosome. Children with Klinefelter syndrome may have smaller testicles that produce less testosterone.
Children with intersex conditions (development of both male and female reproductive organs) may also have trouble with testosterone production.
Pituitary gland disorders
The pituitary gland is a tiny gland found in the brain. It produces, or stimulates the production of, many hormones. In men, it “tells” the testicles to make testosterone. If there is a problem with the pituitary gland, the testicles might not get the “message” to produce.
Trauma
Testicles that have been injured in an accident or through pelvic trauma may not function properly.
Cancer treatment
If a man has one or both testicles surgically removed, his body will produce less testosterone. Chemotherapy and radiation can affect testosterone production, too.
Obesity
Testosterone deficiency is more common in men who are overweight or obese. That’s because fat cells convert testosterone to estrogen, another type of hormone. In addition, obese men may have lower levels of sex hormone binding globulin (SHBG), a substance that carries testosterone through the bloodstream. Weight loss might help restore testosterone levels.
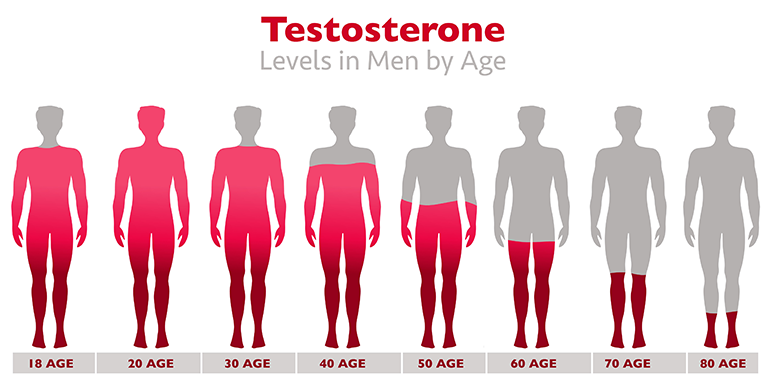
Age
When men reach their thirties, their bodies start producing less testosterone. The decline is gradual—about 1% each year—and might not be noticeable at all. Some people call this change andropause or male menopause, comparing the testosterone decline to the drops in estrogen production in women’s bodies during menopause. However, this comparison is not accurate. Men’s testosterone levels decline gradually, while women’s estrogen levels fall more quickly over time.
Here are some other issues that can contribute to TD:
- Autoimmune disorders
- Infections
- Medications (such as antidepressants, opioids, and narcotics)
- Liver disease
- Kidney disease
- Diabetes
- Metabolic syndrome (high blood pressure, high blood sugar, unhealthy cholesterol levels, excess belly fat)
- HIV and AIDS
How is testosterone deficiency diagnosed?
When diagnosing TD, several factors are considered:
Blood tests
Several substances are checked during blood tests.
Total testosterone
Testosterone circulates in the bloodstream, and it is classified in two different ways. Attached testosterone attaches to proteins in the blood. Free testosterone circulates on its own, not attached to another substance. Most testosterone is attached.
For the purpose of diagnosing TD, doctors assess total testosterone (both attached and free), which is measured in nanograms per deciliter (ng/dL). For context, think of a typical paper clip, which weighs about a gram. A nanogram weighs one-billionth of a gram. A deciliter represents one-tenth of a liter. (To visualize a liter, think of a liter of soda.)
The American Urological Association (AUA) defines a “normal physiologic” testosterone range as 450-600 ng/dL.
For a TD diagnosis, the AUA uses a cutoff of 300 ng/dL. In other words, men whose total testosterone levels are below 300 ng/dL could be diagnosed with TD.
Doctors conduct two blood tests on different days. Both tests are done in the early morning because a man’s testosterone levels fluctuate throughout the day. Levels are usually higher in the morning and lower at night. The protocol of testing in the morning keeps measurements consistent.
Luteinizing hormone (LH)
Produced by the pituitary gland, luteinizing hormone spurs testosterone production by the testes. If LH levels are abnormal, there could be a problem with pituitary gland function or a hormone disorder.
Prolactin
Prolactin is another hormone produced by the pituitary gland. High levels might signal an issue with this gland.
Hemoglobin and hemocrit
Red blood cells contain hemoglobin, a substance that brings oxygen from the lungs to other parts of the body. Hemocrit refers to the percentage of red blood cells found in the blood. High levels of hemocrit could signal polycythemia – an increase in red blood cells that can lead to blood clots. Polycythemia can be a side effect of TD treatment, so it is helpful to get baseline values during diagnosis.
Medical history
Doctors will likely ask about the following:
- Any symptoms associated with low testosterone
- Prescribed medications and use of other drugs
- Past illnesses
- Past traumas, accidents, and surgeries
- Illnesses that run in the family
- Development at puberty
Other assessments
During a physical exam, providers usually check the following:
- BMI (body mass index)
- Waist circumference
- Blood pressure
- Cholesterol and triglyceride levels
- Blood sugar
- Hair patterns
- Testicle size
- Prostate size
- Development of breasts (gynecomastia)
Other tests, if necessary.
Estradiol. If a man has shown some breast development, doctors may check his levels of estradiol, a form of estrogen.
PSA (prostate-specific antigen). Men over age 40 may have their PSA levels checked. High PSA could indicate a prostate condition, such as prostate cancer. Because testosterone replacement therapy, a typical treatment for TD, can be risky for men with prostate cancer, it’s important to screen for prostate cancer before any treatment begins.
How is testosterone deficiency treated?
When considering treatments for TD, we first consider the cause.
When considering treatments for TD, we first consider the cause. If we can pinpoint the reason a man’s testosterone levels are low, treating the underlying condition might be the first step toward improvement. For example, if a man has low testosterone due to obesity, we might suggest weight loss, a healthy diet, and exercise.
Testosterone replacement therapy (TRT) is another option. TRT has 2 goals: to boost testosterone levels into a normal range (usually between 450 and 600 ng/dL) and to relieve the symptoms a patient is experiencing due to his testosterone deficiency. Usually, improvement of symptoms occurs within the first 3 months of treatment.
Testosterone preparations are available by prescription; in fact, testosterone prescribed by a healthcare professional is the only safe way to treat TD. It can be administered in several ways, and we’ll talk with you about your personal situation, medication preferences, insurance coverage, and out-of-pocket costs:
Gels, creams, and patches
These are called transdermal or topical treatments: they are applied to the skin. For example, a man might apply a gel to his belly every day or a patch to his shoulder every few days. Specific instructions are provided. Often, the exact dose is pre-measured in a corresponding pump or tube.
Advantage:
- Application is easy and convenient.
Disadvantages:
- Some men develop rashes or itching from topical testosterone treatments.
- Men need to be careful when using topical testosterone and make sure that the product does not transfer to anyone else, especially women or children.
Men are advised to cover the treatment area and keep products in a safe place, out of reach for children and pets.
Men should also wash their hands thoroughly after applying testosterone. Clothing that has come into contact with testosterone should be washed separately.
Why is avoiding testosterone transfer to others so important? Women who come into contact with topical testosterone may develop unusual hair growth or acne. In pregnant women, testosterone exposure may harm the unborn baby. Exposure in children may lead to enlarged genitals, pubic hair growth, increased sexual desire, increased erections, aggressive behavior, and bone growth issues.)
Injections
Some men go to their doctor’s office to receive testosterone injections. Others self-inject their prescribed medicine at home. Frequency can vary from one injection every week to one injection every 10 weeks. (Most men have an injection every 2 weeks.) Shots may be placed just under the skin or directly into a muscle.
Advantages:
- Injectable testosterone tends to be the most affordable option.
- The dosing schedule may be more convenient.
Disadvantages:
- Testosterone levels can fluctuate. Typically, testosterone levels increase right after the injection, then gradually decrease until the next one. (In some cases, the dosing protocol might be changed to 1 injection once a week to even out the amount of testosterone given over time.)
- Some men might be uncomfortable with the idea of injections.
- Men may still need to travel to a doctor’s office to receive injections.
- Allergic reactions are another potential side effect.
By mouth
This route is also called oral or buccal (buccal is a word that refers to the cheek or mouth cavity and in this case refers to placing a patch between the gum and cheek). Options might include capsules to swallow or patches to place on the gum.
Advantage:
- Taking testosterone by mouth may be less invasive.
Disadvantages:
- Some men experience gum irritation, pain, headache, or a bitter taste in the mouth. Gum disease (gingivitis) is possible as well.
Through the nose (intranasal)
Testosterone in gel form is pumped into the nostril.
Advantage:
- The delivery method is less invasive. One form of intranasal testosterone, Natesto, may have fewer effects on fertility, but more research is needed. See more details below.
Disadvantages:
- Men may need to take their medicine 3 times a day, which could be inconvenient.
- Side effects may include congestion, nasal irritation, scabbing, a runny nose, or changes in smell.
Pellets
Administered by a doctor, pellets are placed under the skin and gradually dissolve. Treatment needs to be repeated every 3 to 6 months.
Advantage:
- The dosing schedule can be convenient. Men do not need to remember to take medication every day or every week.
Disadvantages:
- Testosterone pellets need to be administered at a doctor’s office.
- Administration is more invasive.
- After pellet implantation, some men experience pain, swelling, or bruising.
How often should a man on TRT see his doctor?
About 2 to 4 weeks after starting testosterone therapy, patients need to return for a checkup. At this time, lab results and symptoms are re-assessed. If results are satisfactory, further assessment is recommended every 6 to 12 months.
If necessary, estradiol and PSA levels will also be assessed periodically.
Hematocrit levels may also be monitored. Hematocrit is a measure of the percentage of red blood cells on the blood. As mentioned earlier, polycythemia— excess amounts of red blood cells—is a possible side effect of TRT. Polycythemia can thicken the blood and raise a person’s risk for stroke or blood clots.
If TRT raises testosterone levels but does not improve symptoms, providers may recommend that men stop TRT. It’s possible that the symptoms are not related to TD, and further evaluation could be necessary.
Is it okay to take over-the-counter TRT medications or order them online?
Men should always have TRT under the care of a qualified medical professional.
You might see testosterone supplements at pharmacies, department stores, or online. Are they safe to use?
No, they’re not. And here’s why:
- Supplements are not regulated by the FDA (U.S. Food and Drug Administration). Therefore, the safety of these products cannot be guaranteed.
- Supplements can contain ingredients that interact with other medications you take. This can make you sick.
- Some supplements have ingredients that aren’t listed on the product label, so you might not know exactly what you are getting.
Urologists tailor treatment to a patient’s personal situation, prescribing formulations that are safe and effective for you. We will also monitor your health after you start testosterone therapy, making any adjustments as needed.
Special Concerns
How might testosterone replacement therapy affect a man’s fertility?
Men who wish to father children may wish to consult a reproductive health specialist before starting testosterone replacement therapy.
Testosterone preparations can reduce a man’s levels of follicle-stimulating hormone (FSH), which triggers sperm production. As a result, testosterone therapy could lower sperm count. Men who are hoping to become a father need to carefully consider the risks testosterone replacement therapy may present to fertility.
Depending on the cause of TD, there might be other medications a man can take to raise his testosterone levels. Some examples are aromatase inhibitors (AI), human chorionic gonadotropin (hCG), and selective estrogen receptor modulators (SERM). Sometimes, a combination of these medications is prescribed.
Note: In September 2020, scientists reported that a nasal testosterone preparation called Natesto may have a less negative impact on sperm production. However, more research is needed before this medication can be safely prescribed to men who wish to preserve fertility.
Is TRT linked to prostate cancer?
No, there is no evidence that connects testosterone therapy to prostate cancer. However, a man’s PSA levels might increase during testosterone therapy, so it is important to monitor them.
Is TRT linked to other health risks?
There have been concerns about testosterone therapy and cardiovascular events, like strokes, blood clots, and heart disease. However, it is not definitely known whether TRT raises or lowers risk of cardiovascular problems. Men are encouraged to discuss any heart concerns with their doctor.
The AUA recommends that men who have had a cardiovascular event wait 3 to 6 months before starting TRT.
It should also be noted that low testosterone itself can be a risk factor for cardiovascular disease.
Resources
American Urological Association
Mulhall, J.P., et al.
“Evaluation and Management of Testosterone Deficiency (2018)”
(Published: 2018)
https://www.auanet.org/guidelines/guidelines/testosterone-deficiency-guideline
Videos included with above guidelines:
- What is Testosterone Deficiency: Definition and Diagnosis
- Monitoring and Management the Testosterone Deficient Patient
- Low Testosterone and Cardiovascular Risk
- Fertility Preservation in the Testosterone Deficient Patient
- Testosterone, PSA, and Prostate Cancer
Healthwise
“Nanograms per deciliter (ng/dL)”
(Current as of: June 17, 2021)
https://paleymd.com/patient-education/healthwise/?DOCHWID=stn166036
Hormone Health Network (The Endocrine Society)
“Low Testosterone (Hypogonadism)”
(Last updated: April 2020)
https://www.hormone.org/diseases-and-conditions/low-testosterone
“Pituitary Gland”
(Last updated: January 2019)
https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/glands/pituitary-gland
“Testosterone Treatments”
(Last updated: March 2018)
https://www.hormone.org/your-health-and-hormones/mens-health/testosterone-treatments
“What is Luteinizing Hormone?”
(Last updated: November 2018)
https://www.hormone.org/your-health-and-hormones/glands-and-hormones-a-to-z/hormones/luteinizing-hormone
The Journal for Nurse Practitioners
Luthy, Karlen E., DNP, FNP, et al.
“Comparison of Testosterone Replacement Therapy Medications in the Treatment of Hypogonadism”
(Full-text. Published: 2016)
https://www.npjournal.org/article/S1555-4155(16)30716-4/pdf
The Journal of Sexual Medicine
Lundy, Scott D., MD, PhD, et al.
“Obstructive Sleep Apnea Is Associated With Polycythemia in Hypogonadal Men on Testosterone Replacement Therapy”
(Full-text. Published: April 16, 2020)
https://www.jsm.jsexmed.org/article/S1743-6095(20)30169-7/fulltext
The Journal of Urology
Ramasamy, Ranjith, et al.
“Effect of Natesto on Reproductive Hormones, Semen Parameters and Hypogonadal Symptoms: A Single Center, Open Label, Single Arm Trial”
(Abstract. Published: September 1, 2020)
https://www.auajournals.org/doi/10.1097/JU.0000000000001078
Medical News Today
Johnson, Jon
“Polycythemia: Everything you need to know”
(December 16, 2019)
https://www.medicalnewstoday.com/articles/polycythemia
MedlinePlus.gov
“Hemoglobin Test”
(Page last reviewed: July 31, 2020)
https://medlineplus.gov/lab-tests/hemoglobin-test/
“Klinefelter Syndrome”
(Topic last reviewed: June 5, 2017)
https://medlineplus.gov/klinefeltersyndrome.html
“Prolactin Levels”
(Page last reviewed: December 17, 2020)
https://medlineplus.gov/lab-tests/prolactin-levels/
“Testosterone Levels Test”
(Page last reviewed: December 3, 2020)
https://medlineplus.gov/lab-tests/testosterone-levels-test/
“Testosterone Topical”
(Page last reviewed: December 6, 2021)
https://medlineplus.gov/druginfo/meds/a605020.html
ReproductiveFacts.org (American Society for Reproductive Medicine)
“Testosterone Use And Male Infertility”
(Created: 2015)
https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/testosterone-use-and-male-infertility/
UpToDate
“Patient education: Low testosterone in men (The Basics)”
(Topic retrieved on November 11, 2021)
https://www.uptodate.com/contents/low-testosterone-in-men-the-basics
Urology Care Foundation
“Testosterone Therapy – What You Should Know”
(2020)
https://www.urologyhealth.org/educational-materials/testosterone-therapy
“What is Low Testosterone?”
https://www.urologyhealth.org/urology-a-z/l/low-testosterone
WebMD
Hoffman, Matthew, MD
“Low Testosterone and Your Health”
(Reviewed: February 7, 2021)
https://www.webmd.com/men/what-low-testosterone-can-mean-your-health