Benign Prostatic Hyperplasia (BPH)
What is BPH?
Getting older is inevitable, and it can be hard to accept the way our bodies change. For many older men, that often includes prostate enlargement and, for some, the urinary trouble that goes along with it.
The medical term for an enlarged prostate is benign prostatic hyperplasia (BPH). You might also hear the terms benign prostatic hypertrophy and benign prostate enlargement (BPE).
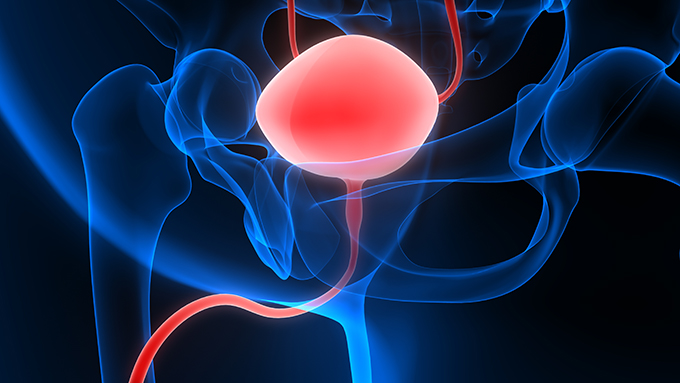
The prostate is a walnut-sized gland found beneath your bladder and in front of your rectum. It makes seminal fluid – the fluid that mixes with sperm when you ejaculate. Running directly through the prostate is the urethra, the tube that allows urine and semen to leave your body.
BPH might become aggravating, but overall, it’s not harmful
BPH becomes more common as you get older. According to UpToDate, an estimated 8% of men between the ages of 31 to 40 have an enlarged prostate. Over age 80, the rate is over 80%.
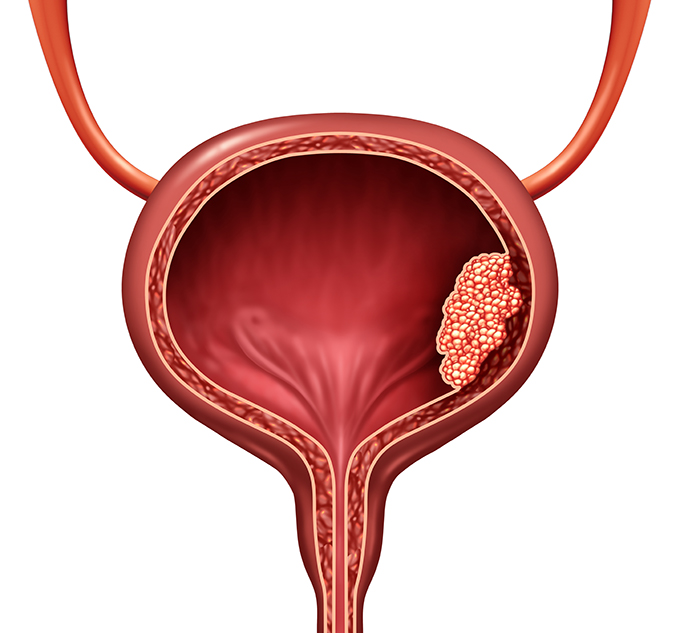
One word that should reassure you is benign. It might become aggravating, but overall, it’s not harmful. And BPH is not the same as prostate cancer. It is possible to have both an enlarged prostate and prostate cancer, but BPH on its own is very common and very treatable.
Symptoms of BPH
While BPH is benign, it can still have some frustrating symptoms, mostly urinary:
- A more urgent and frequent need to urinate. That “gotta go” feeling might be stronger, and it might happen more often.
- Frequent urination at night (nocturia). If you’re waking up every couple hours with the need to pee, that could be a sign of BPH.
- Feeling like your bladder isn’t completely empty, even if the urine flow has stopped.
- Straining during urination. You might feel like it takes more effort – or you have to push – in order to pee.
- Weak urine flow or a flow that stops and starts. You might dribble or leak urine, too.
- Bloody urine (hematuria)
BPH symptoms usually start when a man reaches his 50s. However, not all men with BPH have symptoms. Some have no problems at all. Or if they do, the symptoms don’t bother them.
What happens when the prostate gland grows?
Basically, when the prostate gland gets bigger, it grows inward rather than outward. And this is why urination becomes a problem.
Recall that the urethra goes straight through the prostate gland. That new growth going inward can press against the urethra – squeezing it, if you will. This process narrows the path for urine flow, slowing it down or blocking it altogether.
Should you simply tolerate BPH symptoms, chalking them up to signs of aging? No. For one thing, there are a variety of treatments available, so there’s no reason to suffer with symptoms. Chances are, there’s a treatment that will work for you.
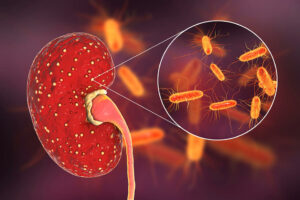
Secondly, not treating BPH can lead to other problems. Your BPH symptoms might worsen over time, eventually damaging your bladder or kidneys.

Diagnosis
Doctors diagnose BPH by taking a medical history and conducting a number of tests. You’ll be asked a lot of questions, and it’s important to be honest. The tests? Some can be uncomfortable. But they’re essential for ruling out other conditions that have similar symptoms:
- Urethral stricture
- Prostate cancer
- Bladder cancer
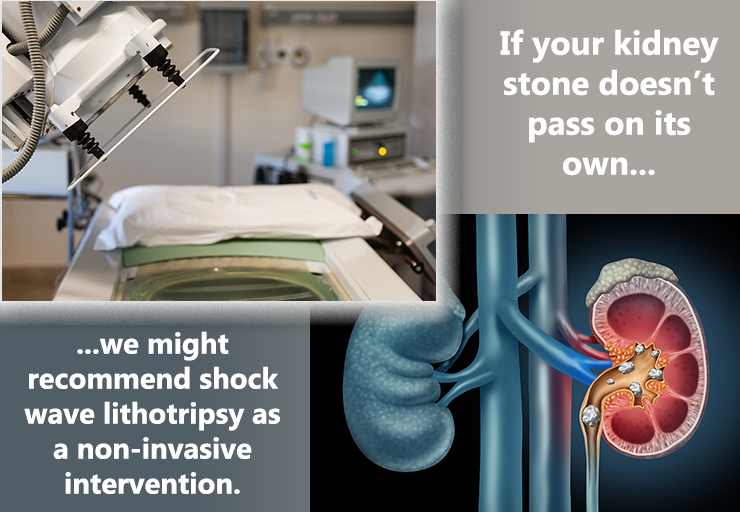
- Kidney or bladder stones
- Overactive bladder
- Neurogenic bladder
Your medical history
Your doctor will want to know about your family medical history and your own experiences with urinary tract infections and prostatitis (inflammation of the prostate). They will also ask you about any over-the-counter products and prescription medications you use. You might want to make a list of these before your appointment. If you use any herbal products or nutritional supplements, make sure you mention those.
The doctor might want to observe you urinating and will likely check your abdomen to see if there are signs of an enlarged bladder.
You might also be asked to complete a questionnaire called the AUA (American Urological Association) Prostate Symptom Index or another assessment tool.
Digital Rectal Exam (DRE)
This exam can be awkward. But it only takes a few minutes, and your doctor can get a lot of useful information.
During a DRE, your doctor will place a lubricated, gloved finger into your rectum. In this way, they doctor can actually feel your prostate gland and assess its size and its texture (lumps, hard spots, soft spots).
A DRE shouldn’t hurt, but you might feel a little uncomfortable. Take some deep breaths, knowing that it will be over soon.
Lab tests
- Urine test (urinalysis). This test is straightforward: You pee into a cup. Your urine sample is then analyzed to see if there is anything unusual.
- Blood tests. In your blood work, your doctor will check your PSA levels. PSA stands for prostate specific antigen. Patients with benign prostatic hyperplasia (BPH) or prostatitis may have larger amounts of PSA.
Other tests
- Urodynamic tests measure the volume and pressure of urine in the bladder and evaluate the flow of urine.
- Uroflowmetry tells the doctor how quickly – and to what extent – you can empty your bladder.
- A pressure flow study can help your doctor determine how much blockage there is.
- A post-void residual (PVR) test measures how much urine stays in your bladder after urination.
- Ultrasonography creates images of your urinary tract to show any abnormalities. Your doctor can estimate the size of your prostate this way, too.
How is BPH treated?
If it turns out you have BPH, you have lots of treatment options. We’ll run through them here, but your doctor will help you decide which one is right for you.
Watchful Waiting
This is a “wait and see” approach. If you’re just starting to have symptoms, or if they’re not bothering you that much, you might not begin treatment right away. Instead, you and your doctor will keep an eye on things. If your symptoms get worse, you can look into other treatments. If they improve (and for some men they do), that’s even better.
While you’re waiting, you can take these steps to get some relief from urinary symptoms:
- Watch your fluid intake. Skip that glass of water at bedtime or if you’re not sure where your next bathroom will be.
- Caffeinated drinks (like coffee, tea, and soda) and alcohol can make you have to “go.” Cut back on these.
- Try to empty your bladder before you going to bed or heading out. If you feel like it’s not completely empty, try again a few minutes later.
- Avoid certain medications, like tranquilizers and over-the-counter cold remedies containing decongestants and antihistamines. These can worsen urinary symptoms.
- Avoid spicy or salty foods.
- Watch your weight and eat a healthy diet.
Medications
Generally, two types of medications are used to treat BPH:
Alpha blockers
If your doctor recommends medication, you’ll probably start with alpha blockers. These drugs open up your urine flow by relaxing smooth muscle tissue, taking some pressure off the urethra.
Examples include terazosin (Hytrin), doxazosin (Cardura), tamsulosin (Flomax), alfuzosin (Uroxatral), and silodosin (Rapaflo).
Alpha blockers can have some side effects, such as headache, dizziness, low blood pressure, fatigue, weakness, and difficulty breathing.
Note: Erectile dysfunction (ED) drugs called phosphodiesterase type 5 (PDE5) inhibitors might interact with alpha blockers. Always check with your doctor if you’re thinking about taking these drugs together.
Alpha-reductase inhibitors
These drugs work by stopping prostate growth. It can take up to 6 months to see how well they work.
Examples include finasteride (Proscar) and dutasteride (Avodart).
Possible side effects are diminished libido, erection or ejaculation problems, depression, breast tenderness or enlargement, and reduced sperm count.
Note: If your partner is pregnant, she should never handle these drugs. Exposure can cause serious side effects for a developing fetus.
Combination Treatments
Some men, especially those with severe cases of BPH or very large prostates, take both alpha blockers and alpha-reductase inhibitors.
What about herbal treatments like saw palmetto?
You might have heard about herbal treatments, particularly one called saw palmetto. However, these aren’t usually recommended. Keep in mind that herbal treatments aren’t regulated by official agencies, like the FDA. And they can interfere with other medications you’re taking. If you’re thinking about any herbal remedies, always check with your doctor first!
Minimally Invasive and Surgical Treatments
If medications aren’t right for you, you doctor might recommend a minimally invasive treatment or surgery. Some of these procedures can be done right in your doctor’s office. Some require a hospital stay. Some men have temporary side effects, like erectile dysfunction (ED). Some men don’t. Your doctor will go over your options. Usually, treatment depends on the size of your prostate, the severity of your symptoms, and your overall health.
Keep in mind that the results of some treatment last longer than others. Ask your doctor if you might need another treatment down the road.
Prostatic Urethral Lift (PUL)
Some doctors call this technique Urolift®. With this procedure, you’ll have either local or general anesthesia. Your surgeon will then use a special needle to position special implants to hold prostate tissue back, away from your urethra. Most men go home the same day as a PUL procedure.
Transurethral Treatments
The word transurethral means “through the urethra.” In other words, excess prostate tissue is removed through your urethra. You might wonder how an enlarged prostate might be accessed through a tiny tube, but doctors use special equipment designed to fit. You’ll be given anesthesia, so you won’t feel a thing.
Transurethral Resection of the Prostate (TURP)
TURP is a common procedure. The AUA estimates that about 150,000 men in the United States undergo TURP every year.
For TURP, you’ll receive general anesthesia. During the procedure, an instrument called a resectoscope is inserted into your urethra. This device has an electrical loop at the end, which removes obstructing prostate tissue and seals blood vessels. An irrigating fluid is used to flush out the debris. Any remaining debris will pass through your urine.
You’ll probably be in the hospital for about 3 days, and you’ll have a catheter to drain urine. During your recovery, you might have some initial discomfort, feel an urgent need to urinate, or have trouble controlling urination. Usually, these symptoms clear up before long.
Some men have sexual problems after TURP, and it might take a year for your sex life to get back to the way it was before the procedure. The most common issue is retrograde ejaculation, sometimes called “dry orgasm” or “dry climax.” You’ll still ejaculate and feel pleasure from orgasm. But semen will travel backward into your bladder instead of forward out of your penis. It eventually passes with your urine. Retrograde ejaculation is harmless, but if you wish to father a child, talk to your doctor first.
Transurethral Incision of the Prostate (TUIP)
If your prostate isn’t greatly enlarged, you might have a TUIP procedure.
Your surgeon will use a laser beam or electrical current to make small cuts in the bladder neck where the urethra joins the bladder, extending into the prostate. This reduces pressure on the urethra.
You might be in the hospital for about 3 days for TUIP, and you’ll probably have a catheter for a few days, too.
Urinary tract infections, retrograde ejaculation, and ED are possible side effects of TUIP, however most issues are temporary. Additional treatment might be necessary in a few years.
(Note: When a laser beam is used, TUIP might be called TULIP (transurethral ultrasound-guided laser incision of the prostate).
Transurethral Electroevaporation of the Prostate (TUVP)
With TUVP, a tool called a resectoscope is inserted into your urethra (after you receive anesthesia). This tool emits an electrical current to destroy prostate tissue. You’ll be in the hospital for one night.
Transurethral Water-Jet Ablation (TWJA)
As the name suggests, TWJA uses strong water jets to destroy extra tissue. It’s a fairly new procedure, and you’ll have general anesthesia. Your hospital stay will likely be just one night, and you’ll need a catheter for about two days. This approach is thought to have fewer sexual side effects.
Transurethral Microwave Thermotherapy (TUMT)
With TUMT, microwaves are used to heat prostate tissue and destroy it. (Don’t worry! There’s a cooling system in place that will protect your urinary tract.) You won’t need anesthesia for TUMT, and you’ll probably go home the same day.
Ablation of the Prostate
Ablation, in BPH terms, means “destroy” excess prostate tissue using electrical, heat, or laser energy. These procedures tend to have less bleeding, and could be more suitable for men with other health issues. Here are some examples:
- Plasma vaporization (“button procedure”). Similar to TURP, but instead of an electrical loop at the end of the device, there are two electrodes.
- Holmium laser enucleation of the prostate (HoLEP). This procedure is also similar to TURP, but uses a holmium laser. You might be in the hospital for a night. And you might experience incontinence afterward, but this usually gets better within 6 weeks.
- Thulium laser enucleation of the prostate (ThuLEP). ThuLEP is similar to HoLEP described above, except a thulium laser is used.
- Holmium laser ablation of the prostate (HoLAP). This procedure is also similar to HoLEP, but the laser vaporizes excess tissue.
- Photoselective Vaporization of the Prostate (PVP). PVP uses a special high-energy laser to vaporize excess prostate tissue. The laser is delivered through an endoscope that’s inserted into your urethra.
The procedure is performed on an outpatient basis, and you’ll likely go home within a few hours. You should still avoid strenuous exercise for 2 weeks afterward, though. - Convective water vapor ablation (CWVA). This technique uses the energy in water vapor (steam) to destroy excess prostate tissue. It’s a same-day procedure that can be done at your doctor’s office, though you might need to use a catheter for a few days afterward. Many men don’t have side effects.
Surgery
Simple prostatectomy
Men who have particularly large prostates or bladder damage may undergo simple prostatectomy – the surgical removal of prostate tissue. Unlike transurethral procedures, prostate tissue is removed through an incision. This incision might be in your lower abdomen (a suprapubic or retropubic prostatectomy). Another option for the location of the incision is your perineum (the area between your rectum and scrotum). This type is called a perineal prostatectomy.
Note: Simple prostatectomy is different from radical prostatectomy
(Note: Simple prostatectomy is different from radical prostatectomy, a procedure used to treat prostate cancer. With radical prostatectomy, the entire prostate gland is removed. Simple prostatectomy just removes a portion of it.)
Nowadays, some prostatectomies are robot-assisted. However, this doesn’t mean that a robot is actually doing your surgery. Your surgeon is still in charge! However your surgeon guides the robot with a computer and follows the action on a monitor. This allows the surgeon to control the robot’s movements with great precision.
You’ll be in the hospital for a few days after an open prostatectomy. Once you’re home, you’ll need to take it easy and avoid any strenuous activity or lifting for a few additional weeks. Depending on the prostate size, many centers with robot-assisted laparoscopic techniques can now perform the surgery using the robot. The advantage of the latter is a shorter hospital stay and earlier recovery.
Some men have incontinence (urine leakage) or erection difficulties after prostatectomy. Your doctor can teach you how to do special exercises called Kegels to strengthen your pelvic floor muscles. Your doctor might also prescribe treatment for erectile dysfunction (ED).