Urinary Tract Infections
Urinary tract infections (UTIs) occur when bacteria (often E. coli) enters your urethra, the tube that carries urine out of the body. Sometimes, the bacteria travels even further into your urinary tract, causing a more severe infection. UTIs can be mild or life-threatening, so it’s important to take them seriously.
To understand UTIs, let’s go over some anatomy first.
Your urinary tract has several components that work together to clear urine from your body. Your kidneys start the process by filtering waste from the blood and producing urine. Next, your ureters transport the urine from your kidneys to your bladder, where it’s stored until you urinate. At that point, urine passes from your bladder to the outside through the urethra.
However, bacteria can make its way up the urethra and into the bladder. It can even travel as far as the kidneys. The result is a urinary tract infection or UTI.
UTIs are common. In fact, the American Urological Association estimates that 8.1 million doctor’s visits each year are due to UTIs.
Types of UTIs
UTIs are categorized in several ways. One way is based on their severity:
- A simple UTI is usually easy to treat. You’ll need to take antibiotics for about three days, maybe a little longer. But you’ll start feeling better after a few doses.
- A complicated UTI is more serious. You’ll need antibiotics for a longer period, and you might even need to begin treatment in the hospital.
Another way to describe UTIs is to use the location of the infection:
- A bladder infection (sometimes called simple cystitis) is just in your bladder. It hasn’t spread outside the bladder.
- A kidney infection (also called pyelonephritis) happens when bacteria has moved past your bladder and into your kidneys. Kidney infections are usually considered complicated or more serious UTIs. Without treatment, a kidney infection can cause permanent damage to your kidney(s). The infection can also spread into the bloodstream and around your body. This can lead to sepsis, a life-threatening condition that can affect multiple organs in your body.
Scientists think that in some cases, the tendency to contract UTIs could be genetic.
UTI Risk Factors
Anyone can get a UTI. But some factors increase your risk:
Being female. UTIs are much more frequent in women. In fact, an estimated 60% of women will get a UTI at some point in their life, while only 12% of men will, according to the American Urological Association.
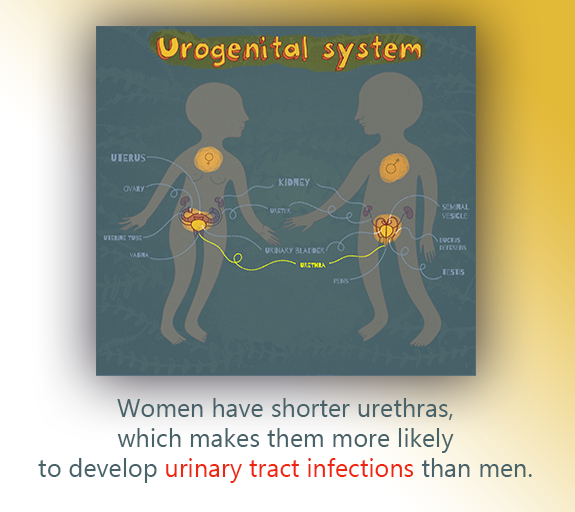
Why? It’s all about anatomy. Women have shorter urethras, so bacteria have a shorter path to the bladder. Also, bacteria like E. coli is found near the anus, which is closer to a woman’s urethra.
Postmenopausal women might be especially prone to UTIs. At menopause, estrogen levels decline. Typically, estrogen can protect from UTIs by promoting antimicrobial substances in the bladder, making tissues less susceptible to infection.
That doesn’t mean men shouldn’t be concerned. Men may have longer urethras, but the bacteria that cause UTIs can also irritate the prostate. For this reason, men with UTIs might need to take antibiotics longer than women do.
A family history of UTIs. Scientists think that in some cases, the tendency to contract UTIs could be genetic.
A medical history of UTIs, kidney stones, or ureteral reflux. If you’ve had a bladder or kidney infection within the past year, you’re more likely to get another one. And you’re at higher risk if you’ve had a urologic condition that alters the way urine flows through your kidneys.
Sexual practices. UTI-causing bacteria can spread from the rectum to the urethra during sex. For example, E. coli can spread to from the rectum to the urethra during intercourse. You might be especially prone to UTIs if you have sex often.
Men who have insertive anal sex are also at higher risk.
Women should be careful about using spermicides for birth control. Some spermicides are thought to kill beneficial bacteria typically found in the vagina. With fewer “good” bacteria available, UTI-related bacteria have more opportunities to grow and spread.
Not being circumcised. Men who have not been circumcised can be more susceptible to UTIs.
Using a catheter or other device. If you’ve had surgery or need a device to help you empty your bladder, there could be more opportunities for bacteria to grow.
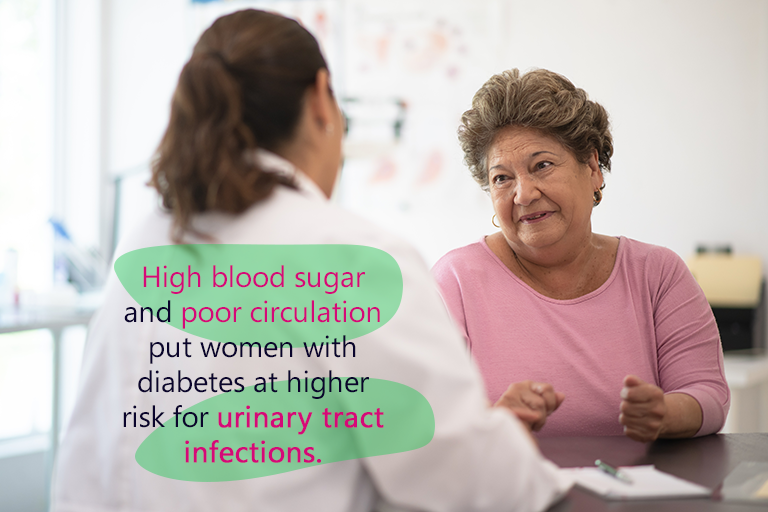
Having certain medical conditions. People with diabetes, an enlarged prostate, or a suppressed immune system are at higher risk for UTIs.
UTI Symptoms
If you have a UTI, you will probably have one or more of the following symptoms:
- Pain or a burning sensation when you urinate.
- A need to urinate more frequently or urgently.
- Low urination flow. You might feel like you really need to “go” but find that very little urine comes out.
- Urine leaks.
- Blood in your urine (also called hematuria).
- Smelly urine.
- Pain in your lower abdomen, pelvic, or lower back.
If you have a kidney infection, you might also have a fever, nausea, and vomiting.

UTI Diagnosis
If you have UTI symptoms, come see us as soon as you can. UTIs can be treated, but it’s better to catch them early before they become more serious. (Note: If you’re pregnant and think you might have a UTI, seek medical attention immediately. Left untreated, a UTI can harm both you and your baby.)
You might not need extensive testing to be diagnosed with a UTI. But certain tests can help us pinpoint the cause of your symptoms and treat them appropriately. Here’s what you might expect:
- Medical history and physical exam. We’ll ask you questions about your symptoms and conduct a urological exam.
- Urinalysis. We’ll take a urine sample and analyze its color, odor, and any bacteria present. We’ll also look for white blood cells. If we find them, we’ll know that your body is fighting an infection. A urinalysis give us details about your infection, which will help us make treatment decisions.
- Urine culture. This is another type of urine test that can tell us about bacteria or yeast in your urine.
UTI Treatment
Bladder infections:
Urinary tract infections are usually treated with antibiotics, such as nitrofurantoin, trimethoprim-sulfamethoxazole or fosfomycin. We might also prescribe a drug called phenazopyridine, which makes urination more comfortable by numbing the bladder and urethra.
Once you start taking antibiotics, you should start feeling better in a day or two. But make sure you take your medicine exactly as we prescribe it for the full duration. That will make it more effective. (If you have any questions or your symptoms don’t improve, give us a call.)
Kidney infections:
Antibiotics are used to treat kidney infections, too. You might take them by mouth at home or receive them as an injection here at our clinic or intravenously (through an IV) at the hospital. We might also suggest acetaminophen or ibuprofen to treat pain and fever. A heating paid might also relieve pain.
Some people get UTIs several times a year
Recurring Bladder Infections
Some people get UTIs several times a year. If this is the case, we’ll conduct further testing. You’ll likely have urinalysis or a urine culture again along with imaging tests like a CT scan, ultrasound, or cystoscopy (a test that allows to see inside your urethra and bladder).
In this situation, we might prescribe different antibiotics:
- Continuous antibiotic therapy. Depending on the medicine, you’ll take pills once daily or a few times a week. Over time, we’ll monitor your symptoms and progress during follow-up appointments. (This may also be called antibiotic prophylaxis. The word prophylaxis refers to a therapy that is used as a preventative measure.)
- Antibiotics after sex. Since sexual activity can raise your risk for UTIs, we might prescribe a special antibiotic to take right after intercourse.
- Antibiotics as needed. We might give you a prescription for antibiotics you can start taking as soon as UTI symptoms start. This way, we can start treating it early. However, you should still tell us about your symptoms. Since UTIs share symptoms with other health problems, we we’ll want to follow up.
We might also recommend cranberry prophylaxis. Research suggests that women with recurrent UTIs may benefit from using cranberry products as a prevention strategy.
Preventing UTIs
There are several steps you can take to lower your risk for UTIs:
- Drink lots of fluids. How much? Experts recommend about 2 liters (a little more than a half-gallon) a day. This keeps your urinary system in good working order.
- Don’t hold your urine. When your body tells you it’s time to urinate, do so at your first opportunity.
- After a bowel movement, wipe from front to back. This reduces the odds of bacteria from the anus coming in contact with the urethra.
- Wash your genitals before sex. Cleansing the area can wash away some bacteria.
- Urinate after sex. Some experts say that this can “flush out” any bacteria that might be making its way up your urinary tract.
- Take showers instead of baths. Bath water might contain bacteria that can reach the urethra.
- Switch birth control methods. Spermicides (used alone or with a diaphragm), can upset the balance of “good” bacteria in the vagina, leaving the area more vulnerable to UTI-causing bacteria. If you use these products, consider another contraceptive method.
- After menopause, consider vaginal estrogen. Some postmenopausal women find it helpful to use vaginal estrogen to lower their risk of recurrent bladder infections.
- Don’t use products that irritate the urethra. Such products might include soaps and feminine hygiene products, like douches.
Resources
American Urological Association
Anger, Jennifer, MD, MPH, et al.
“Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline (2019)”
(2019)
https://www.auanet.org/guidelines/guidelines/recurrent-uti
Centers for Disease Control and Prevention
“What is sepsis?”
(Page last reviewed: August 17, 2021)
https://www.cdc.gov/sepsis/what-is-sepsis.html
MedlinePlus
“Cystoscopy”
(Review date: April 26, 2020)
https://medlineplus.gov/ency/article/003903.htm
“Sepsis”
(Page last updated: June 20, 2021)
https://medlineplus.gov/sepsis.html
“Urinalysis”
(Page last updated: June 9, 2020)
https://medlineplus.gov/urinalysis.html
“Urine culture”
(Review date: October 8, 2018)
https://medlineplus.gov/ency/article/003751.htm
UpToDate.com
Hooton, Thomas M., MD
“Patient education: Urinary tract infections in adolescents and adults (Beyond the Basics)”
(Topic last updated: December 3, 2020)
https://www.uptodate.com/contents/urinary-tract-infections-in-adolescents-and-adults-beyond-the-basics
Urology Care Foundation
“Kidney (Renal) Infection – Pyelonephritis”
(No date provided)
https://www.urologyhealth.org/urology-a-z/k/kidney-(renal)-infection-pyelonephritis
“Urinary Tract Infections in Adults”
(Updated: April 2019)
https://urologyhealth.org/urology-a-z/u/urinary-tract-infections-in-adults
